Between June 1944 and VE-day some 175.000 GIs were admitted to a US Army medical installation in the ETO due to an infectious disease. Only 314 of these men died from these infectious diseases (0,02%). The total number of men admitted to a US Army medical installation for battle injuries in the ETO was 393,987. Of these men, 12,523 died (3.2%).
These were historically low numbers. One of the main reasons for this was the widespread use of antibiotics. The use of antibiotics not only cured infections but also prevented their onset in battle wounds.
During the War, two types of antibiotics were used by the US Army: sulfa drugs and penicillin. Their discoveries, developments, and ultimate use during WW2 are fascinating stories. In this article, I will take a look at the story of antibiotics in the ETO.
Sulfa Drugs.
The term chemotherapy is now used only to describe cancer therapy, but at its origin, the term described a revolutionary new way of thinking about medication: the use of chemicals as medicine.
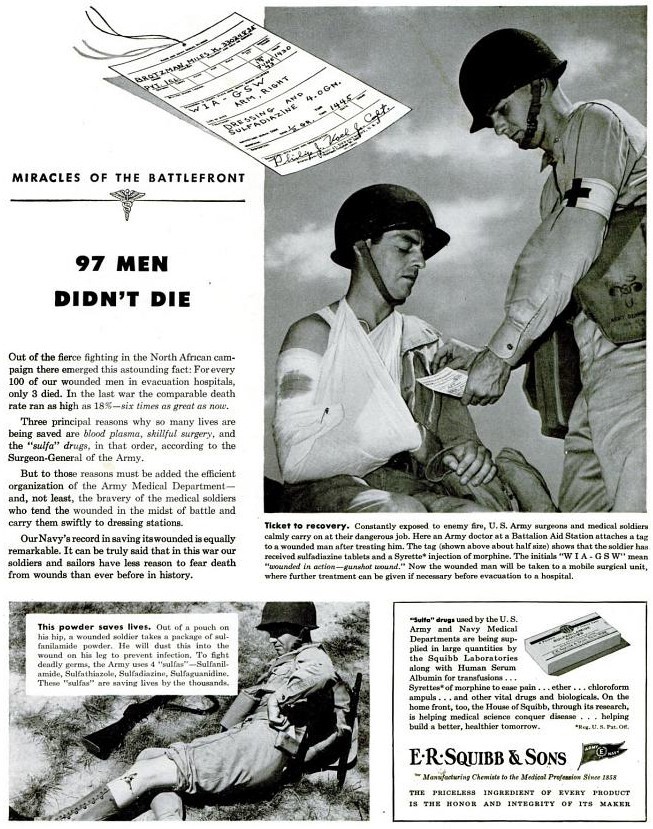
Broadly considered the father of chemotherapy is Paul Ehrlich (1854-1915).
Paul Ehrlich
His research and development of using dyes to stain and then study cells and pathogens led him to conclude that adding chemicals to dyes, that could stain specific cells or pathogens, could affect these cells/ pathogens specifically. So the theory was that the dye “locked in on the target”, the added chemical could then destroy it.
This theory led to a new therapy for syphilis: Salvarsan. In this medicin arsenic was added to a dye that could stain Treponema Pallidum, which caused syphilis.
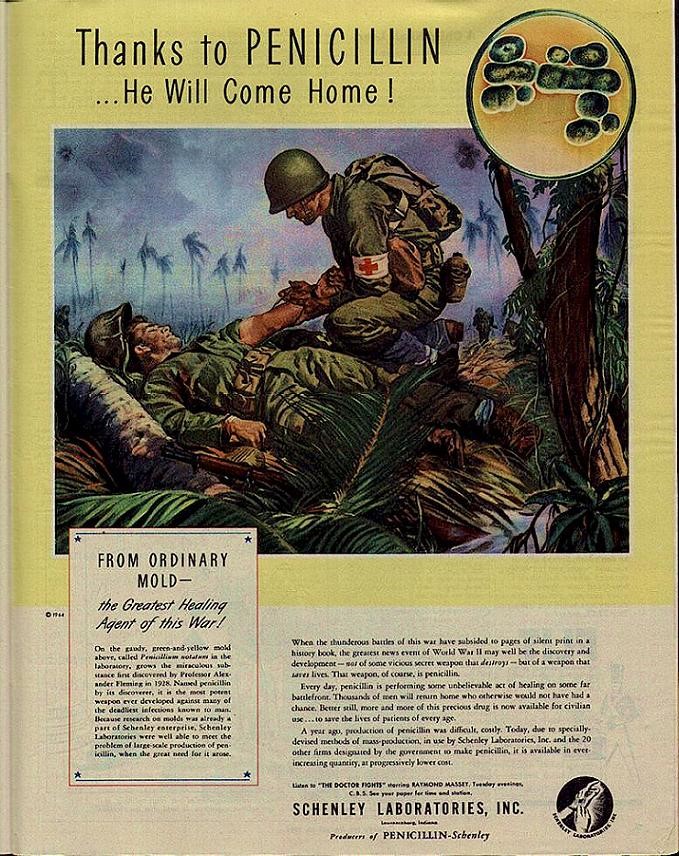
Similarly, Gerhard Domagk (1895-1964) began the development of a new type of medicine.
Gerhard Domagk
He used aniline, a chemical used in dyes that were derived from coal tar, to produce Prontosil in 1932. In 1934 it was first used effectively on patients with Streptococci infections.
Prontosil
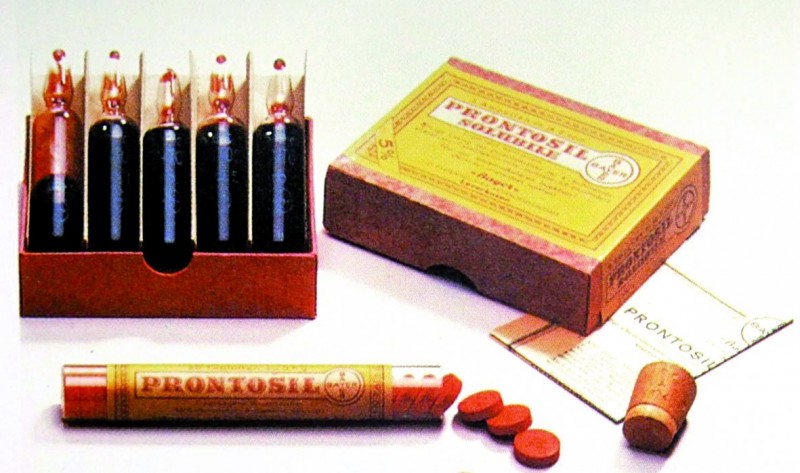
For his discovery, Domagk was awarded the Nobel Prize for Physiology and Medicine in 1939. As he was about to accept this award, the Gestapo forced him to decline it. Their motives for this lay in the award of the Nobel Peace Prize to Carl von Ossietzky, a German pacifist. This award did not fit the Nazi idealogy, making them suspicious of all Nobel Prized. Domagk received his well-deserved award after the War, in 1949.
In 1935, French researchers at the Pasteur Institute discovered that the effective chemical in Prontosil was sulfanilamide and that it did not need the dye chemical to be effective.
Sulfanilamide became the first of the sulfa drugs to be produced as an antibiotic. As this chemical had already been discovered and patented in 1908 by Paul Gelmo, who did not know its antibiotic capabilities, by the time it could be produced as an antibiotic the patent had already expired making it free to be produced by everybody.
In 1936 the son of President Franklin D. Roosevelt was cured of an infectious disease by using sulfanilamide, showing to the American public the effectiveness of this drug, helping greatly in its popularity.
The effect of sulfanilamide being patent-free was unfortunately not only a blessing. In 1937, the S.E. Massengill Co. produced Sulfanilamide in liquid form called Elixer of Sulfanilamide.
Elixer of sulfanilamide
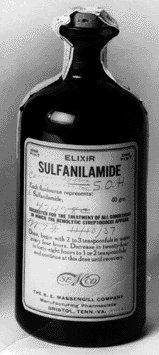
This elixir was a solution of sulfanilamide in Diethylene Glycol, a toxic but sweet-tasting liquid often used as anti-freeze. In September and October 1937 the use of Elixer of Sulfanilamide killed over 100 patients in the US. The shock of this tragedy led directly to new and more strict regulations on drugs in the 1938 Food, Drugs and Cosmetics Act. This act gave the FDA far more authority to regulate the research and development of drugs before they were marketed.
Sulfanilamide does its antibiotic work by blocking the bacteria’s capability to form folic acid, needed to form DNA. So, it hinders the bacteria to multiply. This bacteriostatic effect does not kill the bacteria directly, but it gives the human immune system a far better chance to combat the infection.
From 1938 onwards, many derivatives of sulfanilamide were developed and tested (some say over 5000 different derivatives were tested). They are known as a group as sulfa drugs. By 1942 the US production of sulfa drugs had reached an astounding quantity of 14 million pounds.
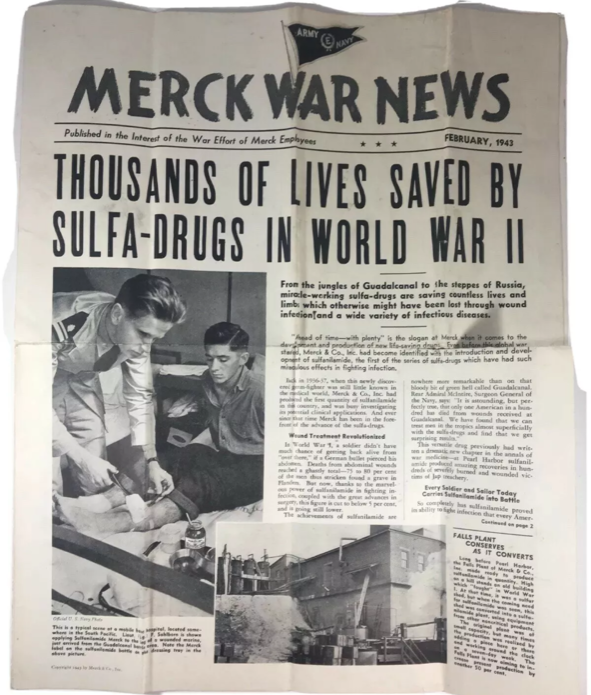
Merck War News, February 1943.
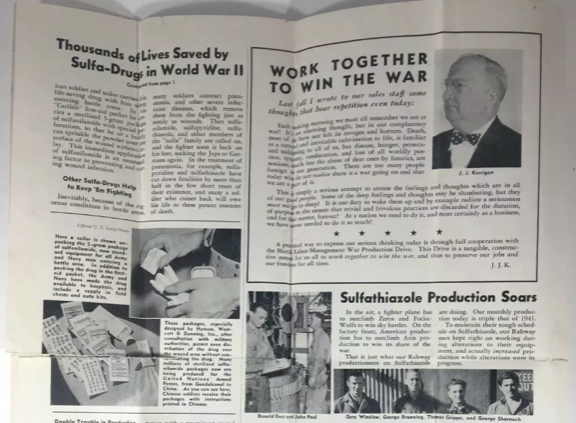
During WW2, the US Army used five different sulfa drugs: sulfanilamide, sulfathiazole, sulfapyridine, sulfadiazine, and sulfaguanidine.
US Army Medical Catalog, 1 March 1944.
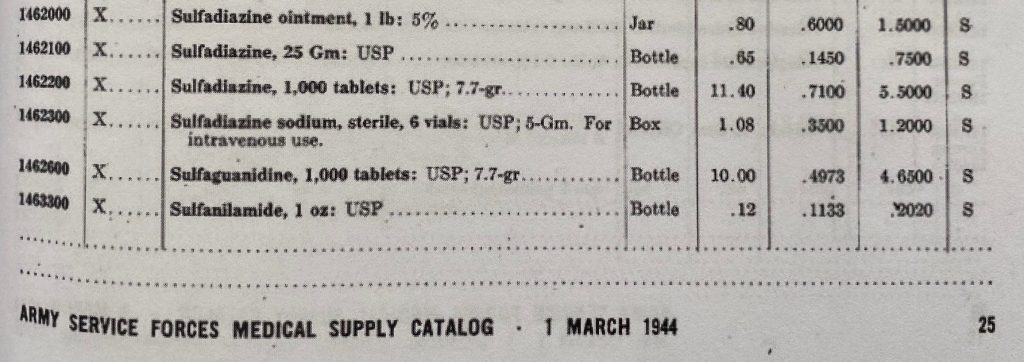
Of these five, sulfadiazine was the most widely used, and for the most infectious diseases. Sulfaguanide was mostly used in bacterial dysentery. Sulfathiazole was mainly used for the treatment of gonorrhea.
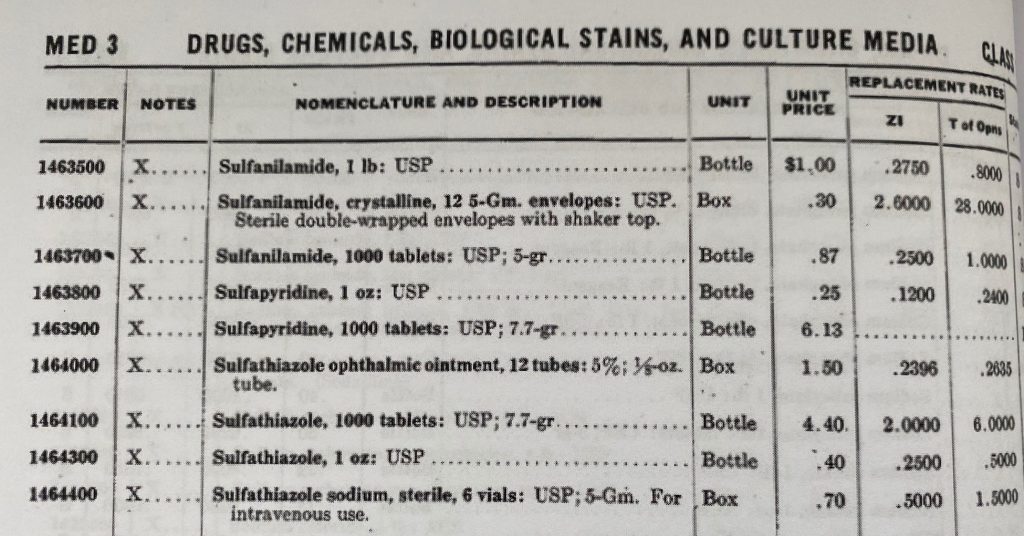
Interestingly, the E-17 survival kit issued to the US Army Air Corps crew contained three types of sulfa drugs.
E-17 survival kit
I have only found one indication for the use of sulfapyridine: the treatment of gonorrhea in sulfathiazole-resistant patients (Sulfapyridine became most famous for the role it played in the treatment of Winston Churchill’s pneumonia in 1943).
Sulfa drugs not only were widely used by the US Army during WW2 for the treatment of many different infectious diseases, but they were also used in the prevention of wound infections. In previous wars wound infections were a major factor in the high mortality rates.
It is quite logical when we think about it: any bullet or piece of shrapnel that caused a wound first had to go through an often dirty, unwashed uniform and penetrate dirty, unwashed skin before it entered a body to cause the wound. This nearly guaranteed wound infections. It makes a lot of sense that, armed with these new medicines, the US Army chose to initiate the treatment or prevention of wound infections as soon as possible. As we can see, the Merck company by 1943 already predicted that “thousands of lives” would be saved by sulfa drugs.
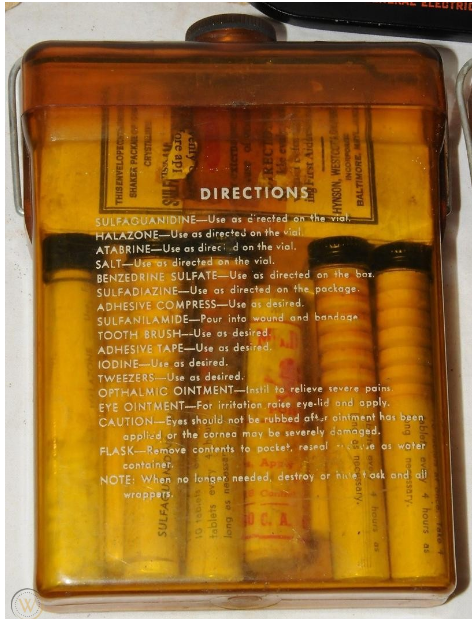
To start immediate treatment, all GIs carried in their first aid kit two items. First, all first aid kits had an envelope or “shaker” containing sulfanilamide powder.
Sulfa powder shaker in First Aid Kit

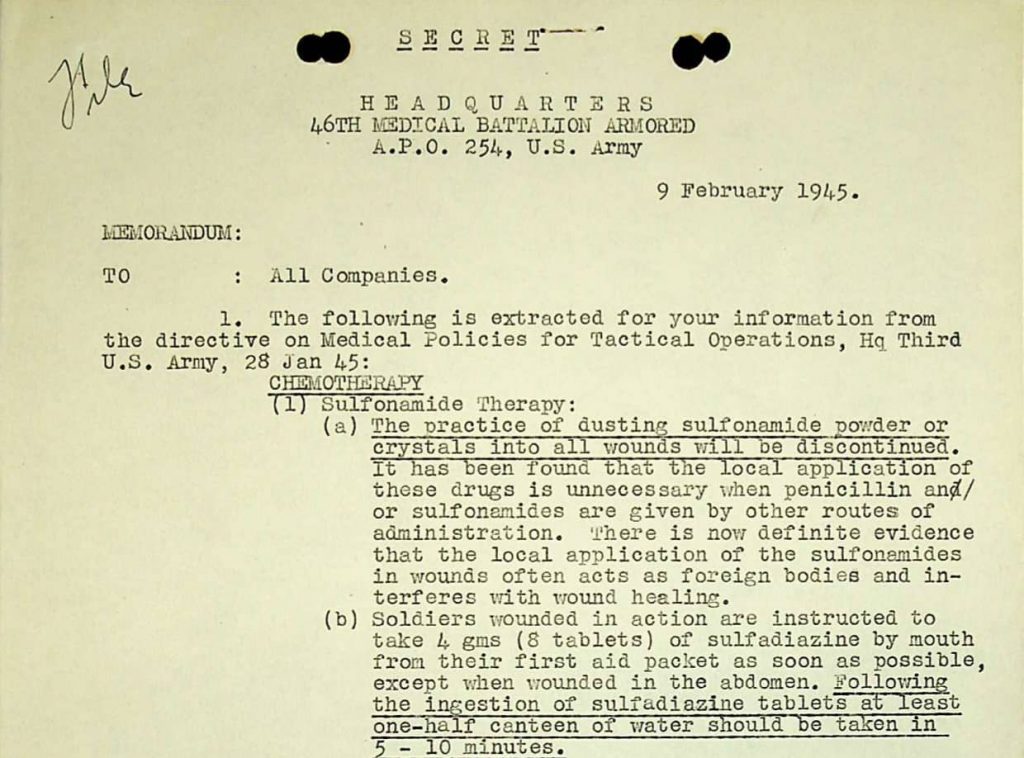
The GIs were instructed to “dust” their wounds with this powder as soon as possible. This use was discontinued in January 1945, when it was discovered that the powder acted as a foreign body (much like a splinter does) in wounds, hindering the healing rather than helping it.
Instructions to stop the use of sulfa powder
Secondly, as we can read in the instructions above, all GIs carried a package of wound tablets. Early in the War, these packages contained 12 tablets of sulfanilamide.
Wound tablets sulfanilamide
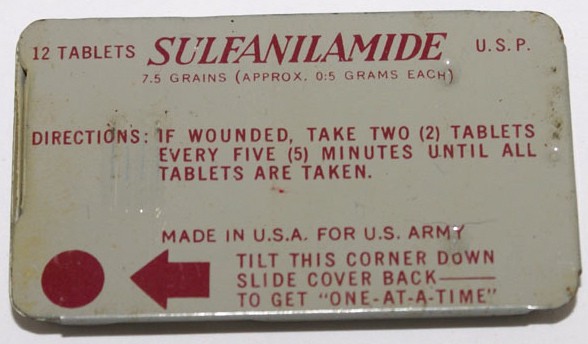
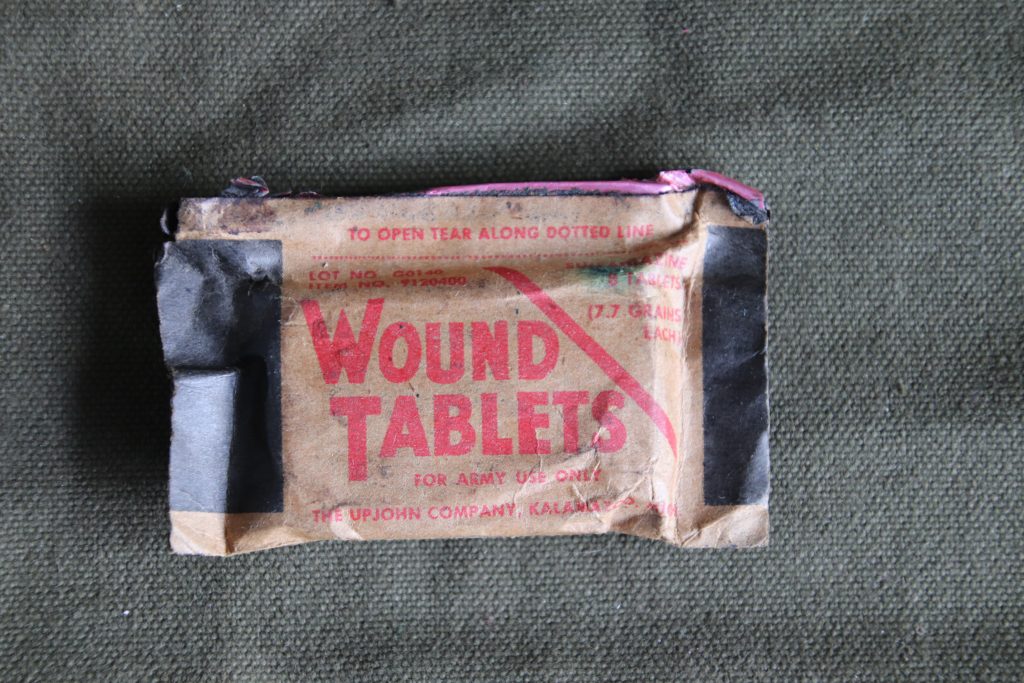
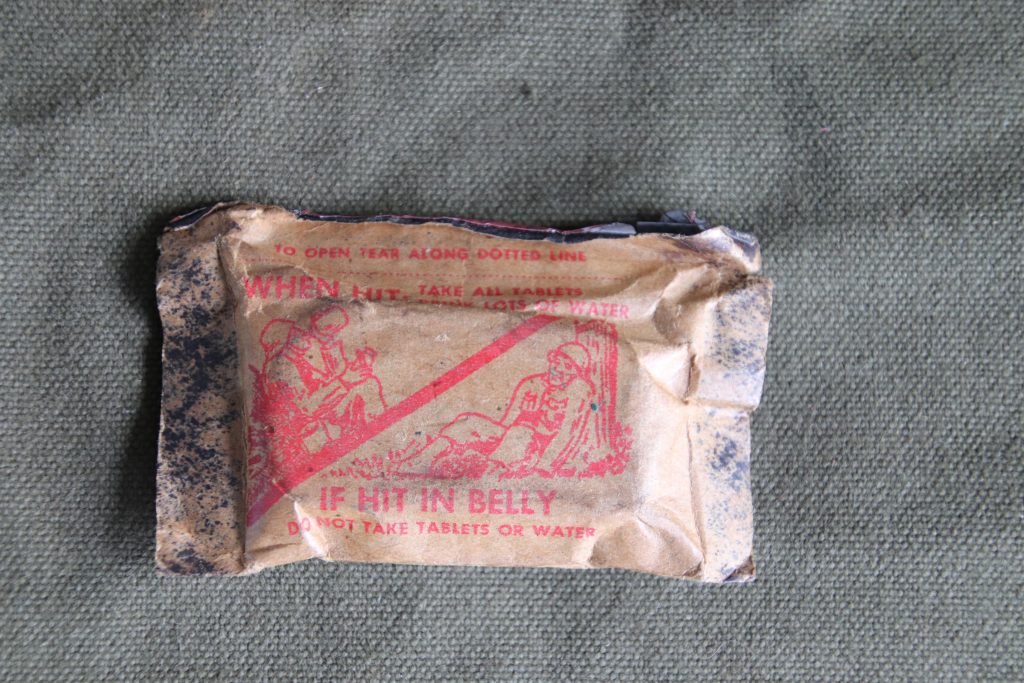
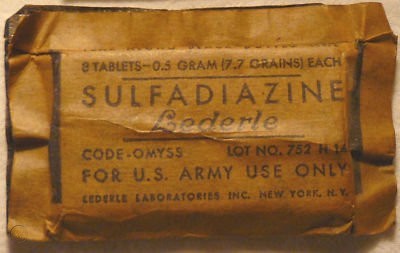
Soon, this was changed to 8 tablets of sulfadiazine. Instructions were to take these tablets with a large volume of water (unless the GI was wounded in the abdomen. Then his instructions were not to take any tablets as sulfa drugs could cause diarrhea as a side effect).
Wound tablets: Upjohn Company, wtih instructions on back.
Wound tablets Lederle Laboratories Inc.
Penicillin.
The story of the discovery of penicillin really starts in November 1921, when Alexander Fleming (1881-1955) had the common cold. He placed some of the mucous produced by this infection on a Petri dish to see which micro-organisms would start to grow. A few days later he found that for some reason some of the micro-organisms started to disappear from the site where he placed the mucous. Other tests conducted with saliva and tears show some of the same results. Fleming concludes that there must be something in these bodily products that can attack micro-organisms. He finally concludes that this must be an enzyme. He calls this lysozyme, an enzyme that can “dissolve” (lysis) these micro-organisms. He discovered that some micro-organisms are affected by lysozyme, but others like staphylococci are not affected by it.
When in September 1928 he returned from a vacation, he found that one of the Petri dishes containing staphylococci had a mold growing on it and that the bacteria were unable to grow near this mold. At first thinking it was another example of lysozyme, it did not draw much attention. But as soon as it became clear that this time the anti-bacterial function was affecting staphylococci, its potential importance became clear. After much testing, it was shown that the mold growing in the Petri-dish was a rather rare type of the penicillium family of molds: Penicillium Notatum.
Fleming tried other, less rare types of penicillium molds, but no other showed the same results. With this knowledge, Fleming started to grow his Notatum strain for further testing. These tests showed that whatever was affecting staphylococci bacteria also affected other Gram-positive bacteria, like streptococci, meningococci, etc. Fleming calls the substance produced by the Penicillium Notatum: penicillin.
The tests showed that the effect was only visible for a short amount of time, proving that penicillin is unstable. Tests on lab animals proved that it is not toxic for these animals.
The fact that these results did not immediately lead to a vast development of penicillin had to do with the difficulties surrounding it: it was not only unstable but producing it in sufficient quantities and of a consistent quality proved extremely difficult. So the medical relevance was not immediately accepted.
This changed when a group of researchers of Oxford University began a program aimed at solving the problems surrounding penicillin.
These researchers were Howard Florey (1898-1968), Ernst Chain (1906-1979), Norman Heatley (1911-2004), Margret Jennings-Fremantle (1904-1994), and Edward Abraham (1913-1999).
Each of these researchers brought their own specific expertise to the team. And despite their many differences and arguments, they played a vital role in making penicillin ready for medical usage.
In 1938, Chain started the research based on Fleming’s publications from ten years earlier. He became convinced that by looking at the problems through the eyes of a chemist, it should not take too long to solve them.
On September 6th, 1939 (five days after the start of WW2) Florey send a request to the Rockefeller Foundation for research funds to make penicillin ready for production within months. On March 1st, 1940 the request was accepted by the Rockefeller Foundation. The team received funds for a three-year research program.
By March 1940 the team had been able to extract penicillin using the freeze-drying technique. This resulted in the first 100 milligrams of penicillin produced, enough to test it on animals twice.
The biggest breakthrough in penicillin research came on May 25th and 26th 1940. On these days the team infected eight mice with harmful streptococci. Four mice were treated with penicillin. Only these four mice remained alive after a few days. (For historical context: this test was conducted around the same time that Operation Dynamo, the evacuation of the BEF at Dunkirk, is initiated).
To test more animals, and to speed up the research, more penicillin needed to be produced. So a major part of the research was directed at finding the best method to do this. By the end of 1940, a new design of ceramic bottles was bought in which the team can grow more Penicillium Notatum.
Starting Christmas 1940, six women began working 24/7 on the production of penicillin. They became known as the “penicillin girls”
Penicillin girls in action.

In January 1941 the first tests on humans could be performed. Albert Alexander was the first patient to be treated with penicillin. At first, his treatment seemed to work well, but when the supply of penicillin ran out he eventually died. These first tests on humans proved that penicillin works. But any future treatment needs to be well-planned and much more penicillin is needed.
In May and June 1941 additional patients were treated (so around the time of Operation Barbarossa, the German invasion of the Soviet Union). We now know that all the penicillin used in tests during 1940 and the first half of 1941 roughly equals a daily dose of penicillin given to patients today.
To find the funds and resources to further expand the production the team was offered a chance by the Rockefeller Foundation to go to the United States, where they arrived on July 6th, 1941.
Here they met with some of the staff of the Northern Regional Research Laboratory (NRRL) at Peoria, Illinois. This meeting resulted in a vast expanse of growing capabilities using the deep fermentation technique.
They also found four pharmaceutical companies willing to participate in the production of penicillin (Merck, Lederle, Pfizer, and Squibb).
In October 1941, the production of penicillin expanded to 50 liters of growing fluid per hour, still not enough to produce penicillin in sufficient quantities for medical use.
On December 7th, 1941 the Japanese Navy attacked Pearl Harbor, bringing the USA into WW2. This changed everything for the production of penicillin. It quickly became a commodity produced under the War Production Board’s supervision. This nearly broke all ties with the British team at Oxford. Penicillin produced in the USA would be sent to the American armed forces, not to the team at Oxford.
The staff at NRRL found a strand of penicillium mold that produced much more penicillin than Penicillium Notatum: Penicillium Chrysogenum which can produce up to 3000 times more penicillin.
In the meantime, Pfizer bought an empty ice factory with plans to use this facility for the production of penicillin. Here 14 deep fermentation tanks of 7,500 gallons each were installed for mass production.
Poster: building the new factory

The new Pfizer factory.

With the find of the new strain of penicillin-producing mold and the improved production capabilities, production started to expand rapidly.
In the first half of 1943, 300 grams were produced (enough to treat just 180 patients), in the second half of 1943 this increased to 15 kilograms.
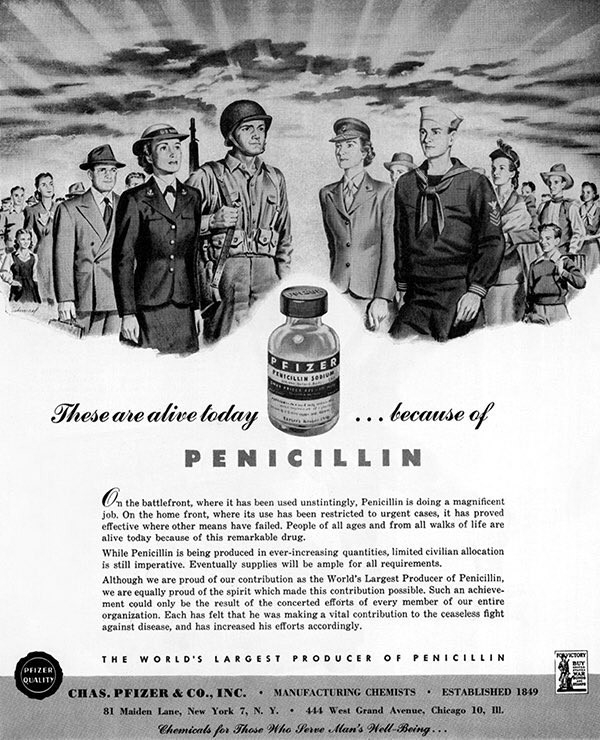
Newspaper July 1943.
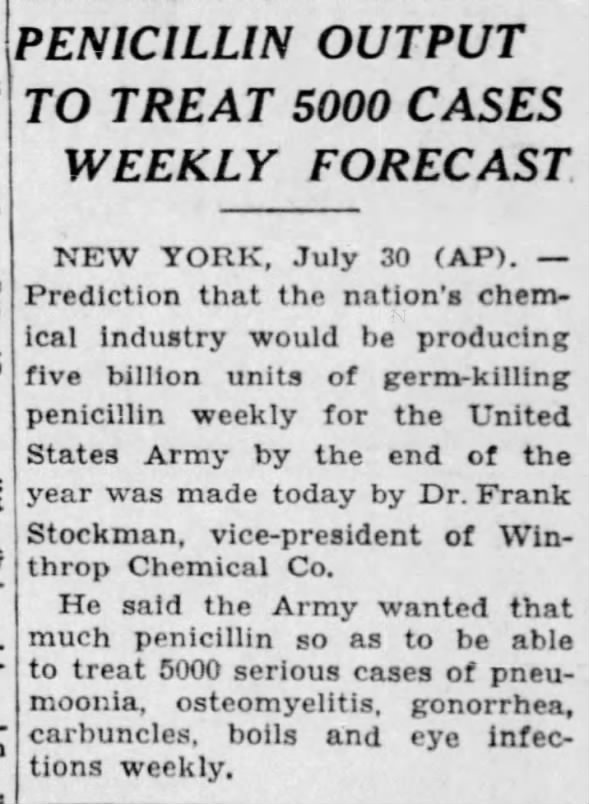
Newspaper Dec 1943.
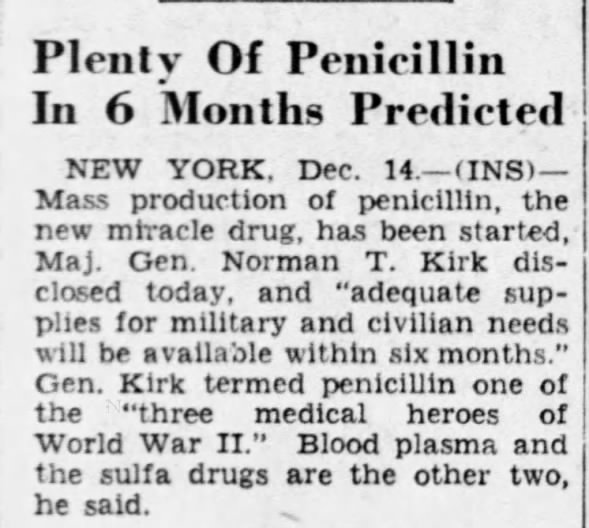
In the months before D-Day production grew to 75 kilograms per month, enough to treat around 40,000 soldiers.
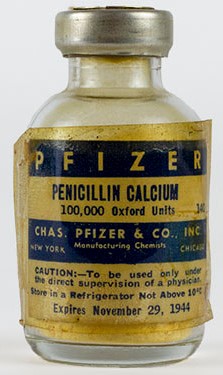
For the invasion of Normandy 300 billion units of penicillin (100,000 units per ampul were needed for a single dose injected) were in stock. The use of units instead of (mili)grams for penicillin started as a way to standardize treatment. As production of penicillin varied between batches, they had to be compared to a known standard unit. At first 5,000 units were placed per glass vial.
Pfizer ampul.
Production figures for 1944 were 1,633 billion units, and for 1945 a total of 7,952 billion units of penicillin were produced.
With the rapidly expanding production of penicillin during the second half of 1943, the US Army Medical Department also expanded its research into the proper use of this new antibiotic.
By January 1944, 28 general hospitals were studying the use of penicillin in surgical infections. Sixteen centers were simultaneously studying its use in sulfanilamide-resistant gonorrhea patients.
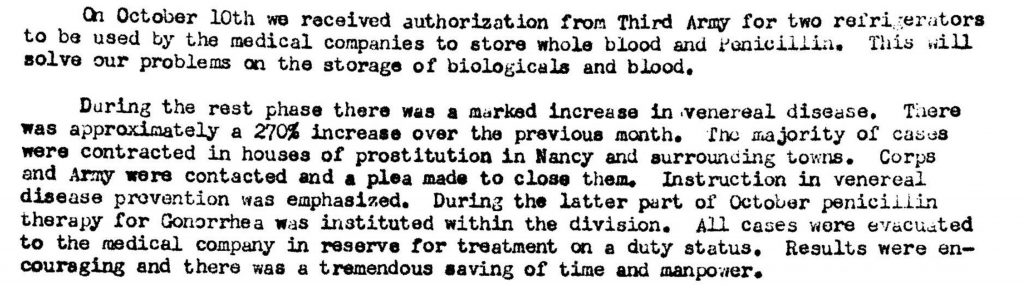
Keeping the US Army Medical Department’s goal of maintaining strength, penicillin soon was used extensively to treat VD patients. Using penicillin not only cured more men than previous treatments, but it also dramatically reduced the time it took to have them ready to return to duty. The previous treatment of gonorrhea using sulfa drugs took 14 to 20 days. With penicillin patients were able to return within 24 hours.
4th Armored Division Surgeon’s report 1944.
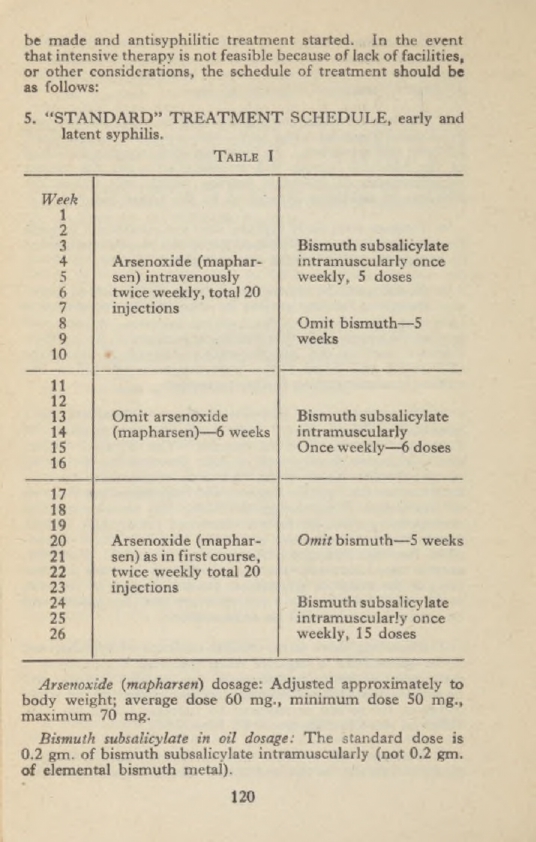
For syphilis patients, the benefits were even greater. The previous treatment using mapharsen and bismuth took 26 weeks.
TM 8-210 Guides of therapy 1942
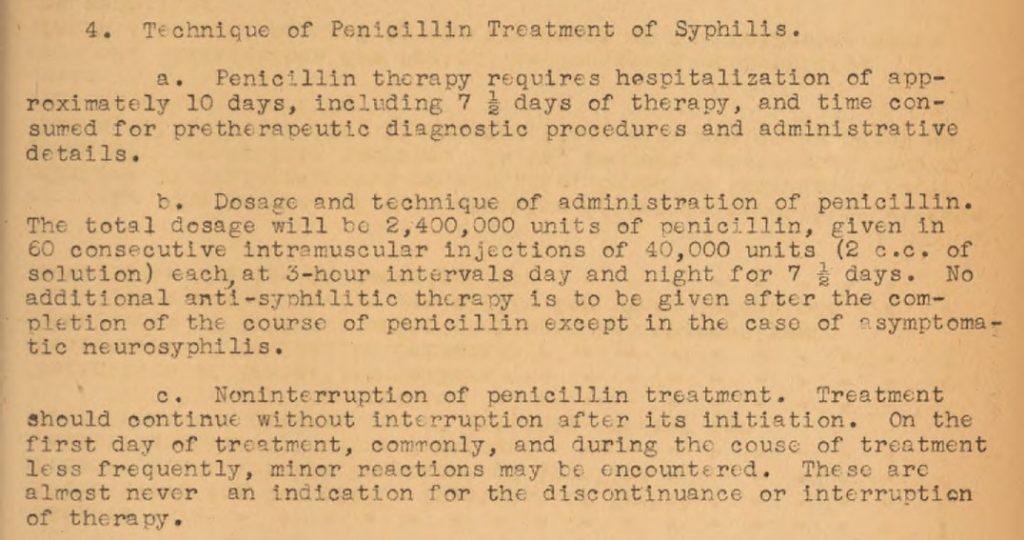
Using penicillin the treatment only took a little over a week.
Within months the use of penicillin became far more widespread as the available supplies increased.
Medical Bulletin ETO no 21. July 1944 pg 2-8 Penicillin Therapy
This bulletin shows that in the first months of the campaigns in the ETO penicillin was used only by hospitals.
By October 1944, the 4th Armored Division received refrigerators at the clearing stations to store whole blood and penicillin. These two items dramatically improved the available medical treatment for severely wounded patients at the second echelon medical installations.
4th Armored Division Surgeon’s Journal.
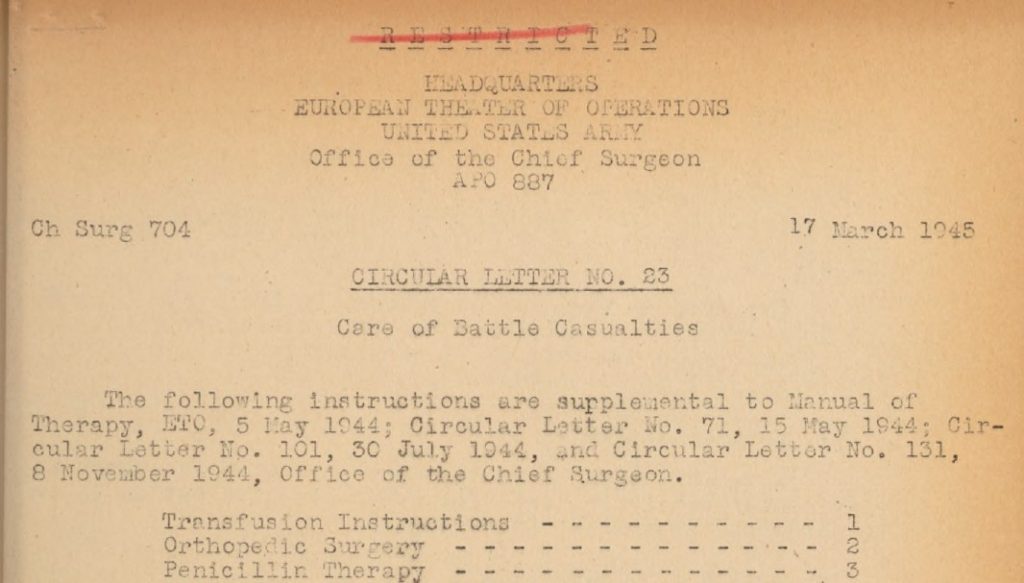
This Medical Bulletin for the ETO of March 23, 1945, shows us that the use of penicillin for almost every wounded man from the clearing stations onwards was the new norm by this date.
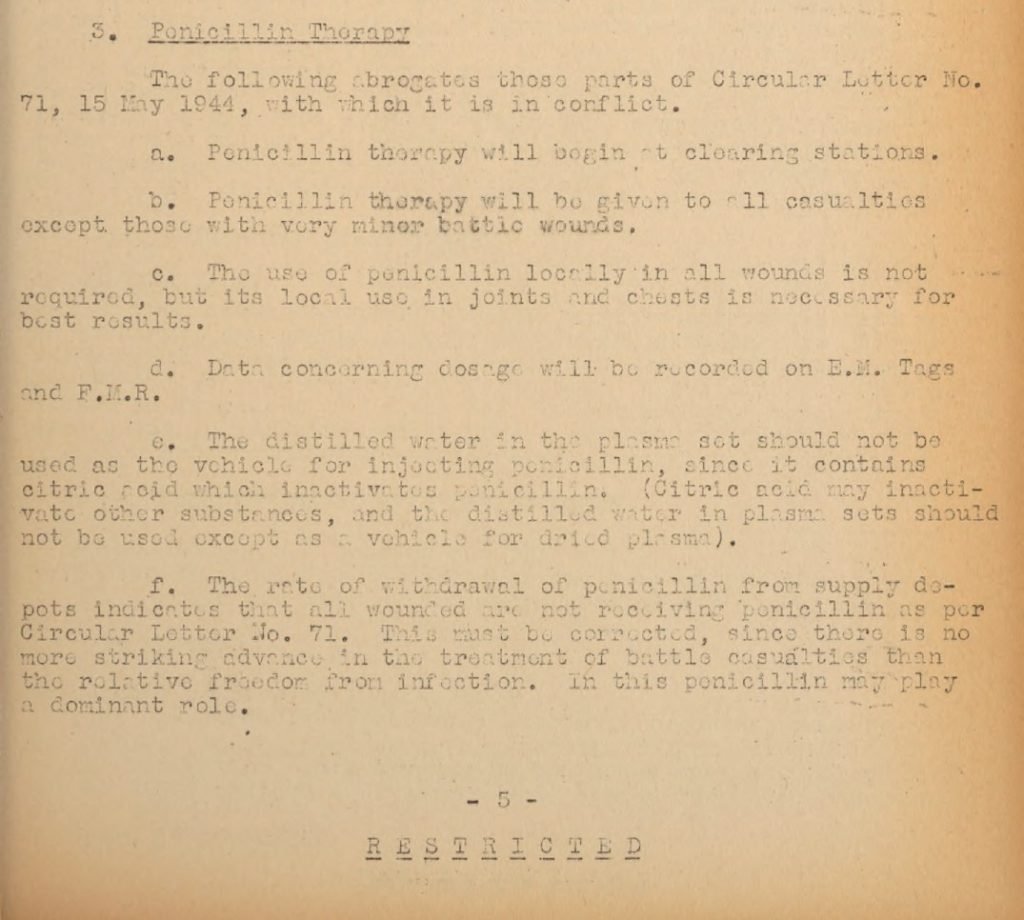
I have found no record of the total amount of penicillin used by the 4th Armored Division’s medics during the campaigns in the ETO. What I did find was the total of units of penicillin used by units in Third Army during WW2:
Penicillin use in Third Army.

The total number of units may seem extremely high, but we must realize that for most treatments a soldier would be given shots of penicillin every 2 hours. This means that on average between 14-24 ampuls, or 1,400,000 – 2,400,000 units, were used per soldier per day.
It is extremely difficult to quantify the gains made in the treatment of soldiers during WW2 by the use of sulfa drugs and penicillin. Comparing statistics from WW1 and WW2 is not easy and often open to misinterpretation. For instance, one might look at the mortality rates of pneumonia patients during both world wars to get an indication of the effects of antibiotics on these rates. Unfortunately, it would be comparing apples and oranges. Most fatalities from pneumonia during WW1 we due to the Spanish Flu pandemic. Only bacterial superinfections in these patients would have been treatable with antibiotics.
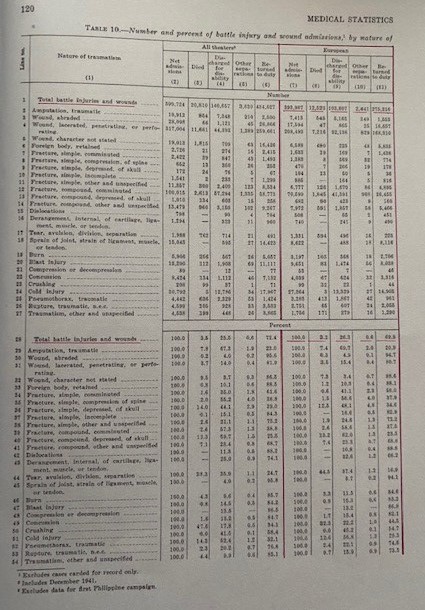
What we can conclude is that according to this article in the Bulletin of the US Army Medical Department of July 1947, the death rate during WW1 was 16.5 per 1000 per annum. For WW2 this had dropped to 0.6 per 1000 per annum. Of all battle casualties who reached the medical installations during WW1 around 8% died. During WW2 this dropped to an average of around 4%.
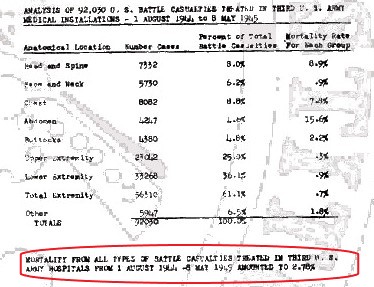
For the ETO this rate was 3.2%. The Third Army After Action Report, Section 17 even claims a rate of 2.78%!
Medical Statistics US Army WW2: battle casualties ETO.
Third Army After Action Report.
This is a dramatic drop in battle casualty death rates, but it is impossible to conclude how much of this decline is specifically due to the use of sulfa drugs and penicillin.
I do think that the Merck newspaper, shown previously in this article, was correct: thousands of lives were saved by the medics of the US Army with the use of antibiotics.